A message from Ms. Delaney about your shoulder rehab:
"Shoulder rehab is not easy. It takes time, effort and dedication from you, the patient, and your physiotherapist as well as everyone around you. Recovery is not a straight-line graph, there are ups and downs, but as long as you put in the effort you will get there in the end. I know this, because I myself have had multiple shoulder surgeries. Yes, that is a photo of me doing my best at my rehab. I've been there. I empathise with you when you are struggling and I celebrate with you when you are making great progress.
Ultimately, the outcome from your shoulder surgery depends on a team effort between me and you. I will give my very best efforts in performing your surgery to the highest possible standard, and then your end of the bargain is to work as hard as you can on your post-op rehab!"
Below are Ms. Delaney's standard post-operative physiotherapy protocols. Each patient is an individual, and protocols will often be tailored to an individual's unique circumstances. These are a general guide to the rehabilitation process from each surgery.
A post-operative shoulder immobiliser is used for certain surgeries, including instability surgery, rotator cuff surgery and shoulder replacements. The DonJoy UltraSling Pro is the most commonly available immobiliser in our hospitals currently. This video shows you how it should be worn:
Additional information can be found at https://www.djoglobal.com/products/donjoy/ultrasling-pro
The UltraSling III may still be used at times. This video explains how to wear it:
Initial Post-op Exercises
Sometimes after shoulder surgery, you will be given gentle passive range of motion exercises to do at home. If you are given these exercises to do, it is important that you continue to do them at home daily after discharge from hospital until you are seen again at our clinic. The hospital physiotherapist will instruct you on these exercises before you are discharge, if they are advised for you by Ms. Delaney. These videos show how these exercises should be done:
1. Passive Forward Flexion (can also be done lying flat on your back):
2. Passive Forward Flexion sitting in a chair (slouch back in the chair):
3. Passive External Rotation:
4. Active-Assisted External Rotation:
Thoracic Spine Exercises
Your thoracic spine has an important role to play in optimising shoulder function. At a certain point during your rehab, it can be beneficial to introduce thoracic spine mobility exercises. Here are some examples of exercises you can do:
1. Easy T-spine
2. Moderate T-spine
3. Advanced T-spine
AC Joint Reconstruction Protocol
AC Joint Reconstruction Protocol (from shoulderdoc.co.uk)
Post op Day 1 - 3 weeks
Level 1 Exercises
Sling for 3 weeks (athletes can wean off sooner under guidance
of club therapist)
Teach axillary hygiene
Teach postural awareness and scapular setting
Core stability exercises as appropriate)
Proprioceptive exercises (minimal weightbearing below 90
degrees)
Active assisted flexion as comfortable
Active assisted external rotation as comfortable
Do not force or stretch
3 - 6 weeks
Level 2-3 exercises
Wean off sling
Progress active assisted to active ROM as comfortable
Do not force or stretch
6 - 12 Weeks
Progress Level 3+ exercises
Regain scapula & glenohumeral stability working for shoulder joint control rather than range
Gradually increase ROM
Strengthen
Increase proprioception through open & closed chain exercise
Progress core stability exercises
Incorporate sports-specific rehabilitation
Plyometrics and pertubation training
Milestones:
Week 6 - Active elevation to pre op level
Week 12 - Minimum 80% range of external rotation compared to
asymptomatic side. Normal movement patterns throughout range
Failure to achieve milestones warrants referral back to surgeon
Return to functional activities
Return to work Sedentary job: as tolerated
Manual job: 3 months
Driving 6-8 weeks
Swimming Breaststroke: 6 weeks
Freestyle: 12 weeks
Golf 3 Months
Lifting Light lifting can begin at 3 weeks. Avoid lifting heavy
items for 3 months.
Contact Sport E.g. Horse riding, football, martial arts, racket sports
and rock climbing: 3 months.
Download protocol as PDF
Bankart Procedure Protocol
Arthroscopic or Open Anterior Stabilisation (Bankart repair) Protocol:
Download PDF
This protocol is intended as a guideline to the post-operative rehabilitation pathway
for a patient who has undergone an arthroscopic or open Bankart repair, it is not intended as a substitute for a Chartered Physiotherapist’s clinical decision-making regarding how the patient is progressing. Clinical exam findings, individual progress, and/or the presence of post-operative complications will determine progress through the pathway. If there are any concerns as to how your patient is progressing, please contact Dublin Shoulder Institute.
Patients are discharged from hospital wearing a Shoulder Immobiliser
(DonJoy Ultrasling III) and with a home exercise programme consisting of
AROM for elbow/ wrist / hand. Patients will then attend for a 2- week post-op
review before attending with their Chartered Physiotherapist.
See above for a video explaining how to correctly wear the shoulder immobiliser can be found here: https://www.dublinshoulder.com/services/shoulder-surgery/
Progression to the next phase is based on Clinical Criteria and/or Time Frames as Appropriate.
Phase I – Immediate Post Surgical Phase (Day 1-21):
Goals:
- Protect the surgical repair
- Reduce pain and inflammation
- Enhance adequate scapular function
- Achieve appropriate range of motion (ROM)
Precautions:
- Remain in sling, only removing for showering and elbow/wrist ROM
- Patient education regarding avoidance of abduction / external rotation activity to avoid anterior inferior capsule stress
- NO Active Range of Motion (AROM) of shoulder
- NO lifting of objects with operative shoulder
- Keep incisions dry and clean until Day 14
Weeks 1-3:
- Sling at all times except where indicated above
- PROM/AROM elbow, wrist and hand only
- Normalize scapular position, mobility, and stability
- Sleep with sling supporting the operative shoulder
- Shower with arm held at the side in an internally rotated position (hand on belly)
- Use ice for pain and inflammation
- Advise patient of low-level kinetic chain exercises ( Bridge, 1 leg bridge, hip hinge)
- Patient education: posture, joint protection, positioning, hygiene, etc.
Phase II – Protection Phase/PROM (Weeks 4 and 5):
Goals:
- Gradually restore PROM of shoulder
- DO NOT over stress healing tissue
Precautions:
- Follow surgeon’s specific PROM restrictions - especially for external rotation
- NO AROM of shoulder or lifting (even though no pain or other symptoms)
Criteria for progression to the next phase:
- Full flexion and internal rotation PROM
- PROM 30 degrees of external rotation at the side
Weeks 4-5
- Continue use of sling until end of week 4 (see patient-specific instructions)
- PROM (gentle), unless otherwise noted by the surgeon
- Full flexion and elevation in the plane of the scapula
- Full internal rotation (hand to belly)
- Glenohumeral joint mobilisations (Grade I/II traction)
- External rotation to 30 degrees at 20 degrees abduction, to 30 degrees at
90 degrees abduction
- Pendulums
- Sub maximal pain free rotator cuff isometrics in neutral
- Continue ice as needed
- Progress kinetic chain where appropriate
- Continue all precautions and joint protection
Phase III – Intermediate phase/AROM (Week 6 - Week 10):
Goals:
- Continue gradual increase of external rotation
- Full AROM
- Independence with ADLs
Precautions:
- Patient to remove sling at 6 weeks post-op if they have not already done so (most arthroscopic Bankart patients will have been instructed to remove at 4 weeks unless hyperlax, very unstable or poor labral tissue).
- NO aggressive ROM / stretching
- NO lifting with affected arm
- NO upper limb strengthening activities
Criteria for progression to the next phase:
- Able to begin gentle external rotation stretching in the 90/90 position
- Full ROM restored in all other planes
Weeks 6 - 10
- PROM (gentle), unless otherwise noted by surgeon- ER to 30-50 degrees at 20degrees abduction, ER to 45 degrees at 90 degrees abduction
- Begin AROM of shoulder - progress to full AROM in gravity-resisted positions
- Begin implementing more aggressive posterior capsular stretching (cross arm stretch, side lying internal rotation stretch)
- Posterior/inferior glenohumeral joint mobilization
- Continue to progress kinetic chain where appropriate
- Enhance pectoralis minor length
- Strengthen scapular retractors
- Use of ice as necessary
Phase IV - Strengthening Phase (Week 10 – Week 16)
Goals:
- Continue to increase external rotation PROM gradually
- Maintain full non-painful AROM
- Normalise shoulder strength, joint stability and muscular endurance
- Gradually progressed activities with ultimate return to full functional activities
Precautions:
- Strenthening to being ONLY after approval by surgeon – timing of strengthening may vary on an individual case-by-case basis and should not be started before almost full ROM has been restored
- DO NOT stress the anterior capsule with aggressive overhead strengthening
- Avoid contact sports/activities
Weeks 10-12
- Continue stretching and PROM of ER to 65 degrees at 20 degrees abduction and PROM of ER to 75 degrees at 90 degrees abduction, unless otherwise noted by surgeon.
- Begin gentle isotonic and rhythmic stabilization techniques for rotator cuff musculature strengthening (open and closed chain)
Weeks 12-16
- Continue stretching and PROM all planes to tolerance
- Continue to progress strengthening programme
- Rehab programme should include sports specific drills where appropriate
Phase V – Return to activity phase (Week 16 - Week 24)
Goals:
- Gradual return to sports activities
- Gradual return to recreational activities
- Gradual return to strenuous work activities
Precautions:
- Do not begin throwing, or overhead athletic moves until 6 months post-op
- Weight lifting:
- Avoid wide grip bench press
- No military press or lat pulls behind the head. Be sure to “always see your elbows”
Weeks 12-16
- Continue progressing stretching and strengthening programme
- Can begin generalized upper extremity weight lifting with low weight, and high repetitions, being sure to follow weight lifting precautions as above
Weeks 16-20
- Can begin golf, tennis (no serving until 6 months.), etc.
- May initiate a cardio strength programme if appropriate
Criteria to return to sports and recreational activities:
- Surgeon clearance
- Pain free shoulder function without signs of instability
- Restoration of adequate ROM for desired activity
- Full strength as compared to the non-operative shoulder (assess using hand held
dynamometry or, if available, isokinetic testing. Collision athletes may have been enrolled in “Shoulder Lab” return to play programme – if so, testing results will be sent to the treating physiotherapist at each stage).
Biceps Tenodesis Protocol
This protocol is intended as a guideline to the post-operative rehabilitation pathway for a patient who has undergone a biceps tenodesis procedure. It is not intended as a substitute for a Chartered Physiotherapist's clinical decision-making regarding how their patient is progressing. Clinical exam findings, individual progress, and/or the presence of post-operative complications will determine progress through the pathway. If there are any concerns as to how your patient is progressing, please contact Dublin Shoulder Institute.
A patient may undergo a biceps tenodesis in conjunction with another procedure such as rotator cuff repair or shoulder arthroplasty – please follow the more conservative rehabilitation protocol, which overrides this biceps tenodesis protocol.
If a subacromial decompression is performed with a biceps tenodesis, again the more conservative rehabilitation protocol is used, which in that case will be the biceps tenodesis protocol.
Patients who have had an isolated biceps tenodesis or a tenodesis with subacromial decompression will be discharged in a simple sling (those who have additionally undergone another reconstructive procedure, such as a rotator cuff repair, will be discharged in a shoulder immobilizer with an abduction pillow, the DonJoy Ultrasling III).
Patients will attend for a 2 week post-op review before attending with their Chartered Physiotherapist.
Progression to the next phase based on Clinical Criteria and/or Time Frames as appropriate.
Phase I – Passive Range of Motion Phase (from 2 weeks post-op)
Goals:
- Reduce shoulder pain and enhance healing process
- Achieve gradual restoration of passive range of motion (PROM)
- Enhance/ensure adequate scapular function
Activity:
- Shoulder pendulum hang exercise
- PROM elbow flexion/extension and forearm supination/pronation
- AROM wrist/hand
- Begin shoulder PROM all planes to tolerance /do not force any painful motion
- Scapular retraction and clock exercises for scapula mobility progressed to scapular isometric exercises
- Sling to be worn while sleeping - support operative shoulder , and place a towel under the elbow to prevent shoulder hyperextension
- Ice for pain relief
- Patient education regarding postural awareness, joint protection, positioning, hygiene, etc.
Precautions:
- No active range of motion (AROM) of the elbow
- No excessive external rotation range of motion (ROM) or stretching. Stop when you feel the first end- feel.
- Use of a sling at all times until 3 weeks post-operatively to minimize activity of biceps ( will be longer if Rotator Cuff procedure was also performed)
- No lifting of objects with operative shoulder
- Keep incisions clean and dry
- NO friction massage to the proximal biceps tendon / tenodesis site
- Advise patient to protect operated arm and limit use even though they may have minimal or no pain.
Criteria for Progression to Next Phase (II):
- Appropriate healing of the surgical incision
- Full PROM of shoulder and elbow
- Completion of Phase I activities without pain or difficulty
Phase II – Active Range of Motion Phase
(start approximately post op week 4)
Goals:
- Reduce pain and enhance healing response
- Achieve gradual restoration of AROM
- Begin waist level functional activities ( light load)
- Wean out of sling by the end of the 2-3 postoperative week
- Can return to light daily activities ( e.g. computer work)
Activity:
- Begin gentle scar massage of anterior axillary incision
- Progress shoulder PROM to active assisted range of motion (AAROM) and AROM all planes to tolerance ( will be easier for patient in supine)
- Age appropriate Kinetic chain exercises (bridge, 1 leg bridge, Hip hinge etc)
- Active elbow flexion/extension and forearm supination/pronation (No resistance)
- Glenohumeral, scapulothoracic, and trunk joint mobilizations as indicated (Grade I - IV) when ROM is significantly less than expected. Mobilizations should be done in directions of limited motion and only until adequate ROM is gained.
- Begin incorporating posterior capsular stretching as indicated
- Cross body adduction stretch
- Side lying internal rotation stretch (sleeper stretch)
- Continued use of ice for pain relief
- Continued patient education: posture, joint protection, positioning, hygiene, etc.
Precautions:
- No lifting with affected upper extremity
- NO friction massage to the proximal biceps tendon / tenodesis site
Criteria for Progression to Next Phase (III):
- Restore full AROM of shoulder and elbow
- Appropriate scapular posture at rest and dynamic scapular control with ROM and functional activities
- Completion of phase II activities without pain or difficulty
Phase III - Strengthening Phase
(start at approximately post-op week 8)
Goals:
- Restore strength, endurance, neuromuscular control
- Return to chest level full functional activities
Activity:
- Continue A/PROM of shoulder and elbow as needed/indicated
- Nearly full elevation in the scapula plane should be acheived before beginning elevation in the other planes.
- Begin rhythmic stabilization drills
- External rotation (ER) / Internal Rotation (IR) in the scapular plane
- Flexion/extension and abduction/adduction at various angles of elevation
- Initiate balanced strengthening program:
- Gain muscular endurance with high repetition of 30-50, low resistance (1-3 lbs)
- Exercises should be progressive in terms of muscle demand / intensity, shoulder elevation, and stress on the anterior joint capsule
- All activities should be pain free and without compensatory/substitution patterns
- Exercises should consist of both open and closed chain activities
- NO heavy lifting should be performed at this time
- Initiate full can scapular plane raises with good mechanics
- Initiate ER strengthening using exercise tubing at 30° of abduction (use towel roll)
- Initiate sidelying ER with towel roll
- Initiate manual resistance ER supine in scapular plane (light resistance)
- Initiate prone rowing at 30/45/90 degrees of abduction to neutral arm position
- Begin subscapularis strengthening to focus on both upper and lower segments
- Push up plus (wall, counter, knees on the floor, floor)
- Cross body diagonals with resistive tubing
- IR resistive band (0, 45, 90 degrees of abduction)
- Forward punch
- Program must include Kinetic Chain and Thoracic mobility exercises
- Use of ice for pain relief as necessary.
Precautions:
- Do not perform strengthening or functional activities in a given plane until the patient has near full ROM and strength in that plane of movement
- Patient education regarding a gradual increase in shoulder activities
- No resisted biceps curls or resisted supination until Phase IV/10 weeks
Criteria for Progression to Next Phase (IV):
- Appropriate rotator cuff and scapular muscular performance for chest level
activities
- Completion of phase III activities without pain or difficulty
Phase IV – Advanced Strengthening Phase
(start at approximately post-op week 10)
Goals:
- Continue stretching and PROM as needed/indicated
- Maintain full non-painful AROM
- Return to full strenuous work activities
- Return to full recreational activities
Activity:
- Continue all exercises listed above ( including Kinetic Chain and T spine mobility)
- Initiate biceps curls with light resistance, progress as tolerated
- Initiate resisted supination/pronation
- Progress isotonic strengthening if patient demonstrates no compensatory strategies, is not painful, and has no residual soreness
- Strengthening overhead if ROM and strength below 90 degree elevation is good
- Continue shoulder stretching and strengthening at least four times per week
- Progressive return to upper extremity weight lifting program emphasizing the larger, primary upper extremity muscles (deltoid, latissimus dorsi, pectoralis major)
- Start with relatively light weight and high repetitions (15-25)
- May initiate pre injury level activities/ vigorous sports if appropriate / cleared by surgeon
Precautions:
- Avoid excessive anterior capsule stress
- With weight lifting, avoid military press and wide grip bench press.
Criteria for return to overhead work and sport activities:
- Clearance from surgeon
- No complaints of pain
- Adequate ROM, strength and endurance of rotator cuff and scapular musculature for task completion
- Continued participation in ongoing home exercise program
Latarjet Procedure Protocol
Download PDF
This protocol is intended as a guideline to the post-operative rehabilitation pathway for a patient who has undergone a Latarjet procedure. It is not intended as a substitute for a Chartered Physiotherapist’s clinical decision-making regarding how the patient is progressing. Clinical exam findings, individual progress, and/or the presence of post-operative complications will determine progress through the pathway. If there are any concerns as to how your patient is progressing, please contact Dublin Shoulder Institute.
Patients are discharged from hospital wearing a shoulder immobiliser (DonJoy Ultrasling III) and with a home exercise programme consisting of AROM for elbow/ wrist / hand. Patients will then attend for 2-week post-op review before attending with their Chartered Physiotherapist.
Please see above for a video explaining how to correctly wear the shoulder immobiliser.
Phase I – Immediate Post Surgical Phase
(Weeks 1- 2)
Goals:
- Minimise shoulder pain and optimize the first phase of bone healing, which involves inflammation (therefore avoid NSAIDS)
- Protect the integrity of the surgical repair
- Begin passive range of motion (PROM) - Forward elevation, scaption, external rotation (ER), internal rotation (IR).
- Enhance/ensure adequate scapular function
Precautions:
- NO active range of motion (AROM) of the operative shoulder
- NO excessive external rotation range of motion (ROM) / stretching. Stop at first
end feel felt and limit overall ER to 30o.
- NO lifting of heavy objects with operated side.
- Remain in sling, only remove for showering or PROM exercises. Shower with arm held at side, forearm resting on belly.
- Keep incisions clean and dry
- Emphasis on NO active use of operated arm even though patient may not be experiencing any pain or other symptoms.
Activity:
- (PROM)/Active-Assisted Range of Motion (AAROM)/ (AROM) elbow and
wrist/hand
- Forward flexion and elevation to tolerance
- Abduction in the plane of the scapula i.e. scaption to tolerance
- Internal rotation (IR) to 45 degrees at 30 degrees of abduction
- External rotation (ER) in the plane of the scapula from 0-25 degrees; begin at
30-40 degrees of abduction; respect anterior capsule tissue integrity with ER
range of motion
- Scapular clock exercises progressed to scapular isometric exercises
- Ball squeezes
- Shoulder Immobiliser to be worn while sleeping - a comfortable sleep position is where patient is quarter-turned with pillow vertical behind operated shoulder.
- Frequent use of ice for pain and inflammation.
- Patient education regarding posture, sling fit, joint protection, positioning, hygiene, etc.
Criteria for progression to next phase (II):
- Adherence to the precautions and immobilization guidelines
- Achieved at least 100 degrees of passive forward elevation and 30 degrees of
passive external rotation at 20 degrees abduction
- Completion of phase I activities without pain or difficulty
Phase II – Intermediate Phase/ROM
(approximately Week 3-8)
Goals:
- Minimize shoulder pain and optimize inflammatory response
- Protect the integrity of the surgical repair
- Achieve gradual restoration of (AROM)
- To be weaned from the sling by the end of week 3.
- Begin light waist-level activities
Precautions:
- NO active movement of shoulder until adequate PROM with good mechanics
- NO lifting using operated arm
- NO excessive external rotation ROM / stretching
- NO activities or strengthening exercises that place an excessive load
on the anterior capsule of the shoulder joint (i.e. no pushups, pec flys, etc..)
- DO NOT perform scaption with internal rotation (empty can) during any stage of
rehabilitation due to the possibility of impingement
Early Phase II (approximately week 4):
- Progress shoulder PROM (do not force any painful motion)
- Forward flexion and elevation to tolerance
- Scaption to tolerance
- IR to 45 degrees at 30 degrees of abduction
- ER 0 - 30 degrees; begin at 30-40 degrees of abduction; respect anterior
capsule tissue integrity with ER range of motion; seek guidance from
intraoperative measurements of external rotation ROM)
- Glenohumeral joint mobilizations as indicated (Grade I, II) – Traction/PA mobilizations should be done in direction of limited ROM.
- Address scapulothoracic and trunk mobility limitations. Scapulothoracic and
thoracic spine joint mobilizations as indicated (Grade I, II, III) when ROM is
significantly less than expected. Mobilizations should be done in directions of
limited movement and only until adequate ROM is gained.
- Begin incorporating posterior capsular stretching as indicated
- Cross body adduction stretch
- Use of ice as needed. Heat can also be used prior to exercises.
- Continued patient education: posture, joint protection, positioning, hygiene, etc.
Exercises for the Kinetic chain should commence by week 4 post-op. Bodyweight lunges (frontal/sagittal plane), hip hinge, single leg stability, bridge/single leg bridge are appropriate. Consideration should also be given to good thoracic spine mobility.
Late Phase II (approximately Week 6):
- Progress shoulder PROM (do not force any painful motion)
- Forward flexion, elevation, and abduction in the plane of the scapula to
tolerance
- IR as tolerated at multiple angles of abduction
- ER to tolerance; progress to multiple angles of abduction once >/= 35 degrees
at 0-40 degrees of abduction
- GH and scapulothoracic joint mobilizations as indicated (Grade I-IV as
appropriate)
- Progress to AA/AROM activities of the shoulder as tolerated with good shoulder
mechanics (i.e. minimal to no scapulothoracic substitution with up to 90-110
degrees of elevation.)
- Begin rhythmic stabilization drills
- ER/IR in the scapular plane
- Flexion/extension and abduction/adduction at various angles of elevation
- Continue AROM elbow, wrist, and hand
- Strengthen scapular retractors and upward rotators
- Initiate balanced AROM / strengthening program
- Initially in low dynamic positions
- Gain muscular endurance with high repetition of 30-50, low resistance 1-3 lbs)
- Exercises should be progressive in terms of muscle demand / intensity, shoulder elevation, and stress on the anterior joint capsule
- Nearly full elevation in the scapula plane should be achieved before beginning elevation in other planes
- All activities should be pain free and without substitution patterns
- Exercises should consist of both open and closed chain activities
- No heavy lifting or plyometrics should be performed at this time
- Initiate full can scapular plane raises to 90 degrees with good mechanics
- Initiate ER/IR strengthening using exercise tubing at 0° of abduction (use towel roll)
- Initiate sidelying ER with towel roll.
- Initiate manual resistance ER supine in scapular plane (light resistance)
- Stretch IR (hand behind back, use towel).
- Initiate prone rowing at 30/45/90 degrees of abduction to neutral arm position
- Kinetic chain exericses
- Ice/Heat as needed
- Continued patient education: posture, joint protection, positioning, hygiene, etc.
Ensure good thoracic spine mobility
Criteria for progression to next phase (III):
- Passive forward elevation at least 155 degrees
- Passive ER in varying levels of abduction
- Passive ER at least 75 degrees at 90 degrees abduction
- Active forward elevation at least 145 degrees with good mechanics
- Appropriate scapular posture at rest and dynamic scapular control with ROM and
functional activities
- Completion of phase II activities without pain or difficulty
Phase III - Strengthening Phase
(approximately Week 8– Week 15)
Goals:
- Normalize strength, endurance, neuromuscular control
- Return to chest level full functional activities
- Gradual and planned build-up of stress to anterior joint capsule
Precautions:
- Do not overstress the anterior capsule with aggressive overhead activities /
strengthening
- Avoid contact sports/activities until at least week 16
- Do not perform strengthening or functional activities in a given plane until the
patient has near full ROM and strength in that plane of movement
- Patient education regarding a gradual increase to shoulder activities
Activity:
- Continue A/PROM as needed/indicated
- Strength program should include PULL – horizontal rows, row on all fours / incline plank (start with light load)
- Initiate gradually progressed strengthening for pectoralis major and minor (PUSH movements) avoid positions that excessively stress the anterior capsule
- Progress subscapularis strengthening to focus on both upper and lower segments
- Push up plus (wall, counter, knees on the floor, floor)
- Cross body diagonals with resistive tubing
- IR resistive band (0, 45, 90 degrees of abduction)
- Forward punch
- Integrate kinetic chain with the above exercises.
Criteria for progression to next phase (IV):
- Passive forward elevation is within normal range
- Passive external rotation at all angles of abduction is within normal range
- Active forward elevation is within normal range with good mechanics
- Appropriate rotator cuff and scapular muscular performance for chest level
activities
- Completion of phase III activities without pain or difficulty
Phase IV - Overhead Activities Phase / Return to activity phase
(approximately Week 16-20)
Goals:
- Continue stretching and PROM as needed/indicated, focus on IR (hand behind back).
- Maintain full non-painful AROM
- Return to full strenuous work activities where relevant.
- Return to full recreational activities
Precautions:
- Avoid excessive anterior capsule stress
- AVOID tricep dips, wide grip bench press; no military press
or lat pulls behind the head. Be sure to “always see your elbows”
- Do not begin throwing, or overhead athletic moves until 16 Weeks post-op or
cleared by surgeon.
Activity:
- Continue all exercises listed above
- Progress isotonic strengthening if patient demonstrates no compensatory
strategies, is not painful, and has no residual soreness
- Strengthening overhead if ROM and strength below 90 degree elevation is good ( Cable Rows/ overhead press)
- Progressive return to upper extremity weight lifting program emphasizing the
larger, primary upper extremity muscles (deltoid, latissimus dorsi, pectoralis
major). Start with relatively light weight and high repetitions (15-25)
- Can do push-ups as long as the elbows do not flex past 90 degrees
- Can do plyometrics/interval sports program if appropriate/cleared by physio and surgeon
- Can begin generalized upper extremity weight lifting with low weight, and high
repetitions, being sure to follow weight lifting precautions.
- May initiate pre injury level activities / vigorous sports if appropriate / cleared by surgeon
Criteria to return to overhead work and sport activities:
- Clearance from surgeon
- No complaints of pain or instability
- Adequate ROM for task completion
- Full strength and endurance of rotator cuff and scapular musculature for task
completion
- Regular completion of continued home exercise program
Pectoralis Major Repair Protocol
Pectoralis Major Repair Protocol:
Pre-op
- ROM Exercises; should have full range of motion pre-op • Maximise shoulder strength of deltoid, intact cuff muscles and scapula stabilisers.
Day 1 - 3 weeks
- Shoulder immobiliser
- Closed chain exercise as tolerated
- Passive / Active Assisted ROM in safe zone (30 degree lateral rotation, 90 flxn, no extn) as tolerated • Do not force or stretch • Avoid pendular exercises and stick exercises • Wrist/hand/finger exercises • Elbow flex/ext, pro/supination • Scapula setting exercises • (Level 1 Exercises)
3-6 weeks:
- Do not force or stretch
- Gentle isometric exercises in neutral as pain allows • Wean off sling • Progress to Open Chain Exercises in safe zone (30 degree lateral rotation, 90 flexion, no extension) as tolerated • Do not force or stretch
- Avoid pendular exercises and stick exercises • (Level 2 Exercises)
6 weeks +:
- Progress to open chain exercises in all ranges as tolerated • motor control prior to any progressive graded resistance • sports-specific rehabilitation • Avoid hyperextending in bench press or flys or pec-deck.
- Avoid high weights with low reps and warm up slowly • (Level 3 Exercises)
Posterior Labral Repair Protocol
Download PDF
Arthroscopic Posterior Labral Repair/Posterior Stabilisation Protocol:
This protocol is intended as a guideline to the post-operative rehabilitation pathway for a patient who has undergone an arthroscopic reverse Bankart repair, It is not intended as a substitute for a Chartered Physiotherapist’s clinical decision-making regarding how the patient is progressing. Clinical exam findings, individual progress, and/or the presence of post-operative complications will determine progress through the pathway. If there are any concerns as to how your patient is progressing, please contact Dublin Shoulder Institute.
Patients are discharged from hospital wearing a Shoulder Immobiliser
(DonJoy Ultrasling III) and with a home exercise programme consisting of AROM for elbow/ wrist / hand. The immobiliser should ideally be positioned with the cushion around by the patient’s side in order to hold the shoulder in neutral rotation or slight external rotation (avoid an internally rotated resting position).
Patients will then attend for a post-op review approximately two to three weeks after surgery before attending with their Chartered Physiotherapist.
Progression to the next phase is based on Clinical Criteria and/or Time Frames as Appropriate.
Phase I – Immediate Post Surgical Phase (Day 1-21):
Goals:
- Protect the surgical repair
- Reduce pain and inflammation
- Enhance adequate scapular function
- Achieve appropriate range of motion (ROM)
Precautions:
- Remain in sling, only removing for showering and elbow/wrist ROM
- Patient education regarding avoidance of abduction/ internal rotation activity to avoid anterior inferior capsule stress
- NO Active Range of Motion (AROM) of shoulder
- NO lifting of objects with operative shoulder
- Keep incisions dry and clean until Day 14
Weeks 1-3:
- Sling at all times except where indicated above
- PROM/AROM elbow, wrist and hand only
- Normalize scapular position, mobility, and stability
- Sleep with sling supporting the operative shoulder
- Shower with arm held atthe side in a neutral position. Avoid hand on belly position
- Use ice for pain and inflammation
- Advise patient of low-level kinetic chain exercises where appropriate (bridge, single leg bridge, hip hinge)
- Patient education: posture, joint protection, positioning, hygiene, etc.
Phase II – Protection Phase/PROM (Weeks 4 and 5):
Goals:
- Gradually restore PROM of shoulder
- DO NOT over stress healing tissue
Precautions:
- Follow surgeon’s specific PROM restrictions - internal rotation to be limited to 30o until 6 weeks post op
- AROM usually allowed to start at 4 weeks post op when weaning out of sling
- NO lifting (even if no pain or other symptoms)
Criteria for progression to the next phase:
- Full flexion and external rotation PROM
- PROM 30o of internal rotation at 20o abduction
Weeks 4-5
- Continue use of sling until end of week 4 (see patient-specific instructions)
- PROM (gentle), unless otherwise noted by the surgeon
- Full flexion and elevation in the plane of the scapula
- Full external rotation – as comfortable.
- Glenohumeral jointmobilisations (Gd I/II traction)
- Internal rotation to 30o at 20o abduction, to 30o at 90o abduction
- Pendulums
- Sub maximal pain free rotator cuff isometrics in neutral
- Continue ice as needed
- Progress kinetic chain where appropriate
- Continue all precautions and joint protection
Phase III – Intermediate phase/AROM (Week 6 - Week 10):
Goals:
- Continue gradual increase of internal rotation
- Full AROM
- Independence with ADLs
Precautions:
- Patient to remove sling at six weeks post-op if they have not already done so (see patient-specific instructions, typically four weeks in sling but in some cases six weeks)
- NO aggressive ROM / stretching
- NO lifting with affected arm
- NO upper limb strengthening activities
Criteria for progression to the next phase:
- Able to begin gentle internal rotation stretching in the 90/90 position
- Full ROM restored in all other planes
Weeks 6 - 10
- PROM (gentle), unless otherwise noted by surgeon: internal rotation to 30-50o at 20o abduction, internal rotation 45o at 90o abduction
- Begin AROM of shoulder:progress to full AROM in gravity resisted positions
- Begin implementing more aggressive posterior capsular stretching: side lying internal rotation stretch/”sleeper stretch” (only if tolerated from pain perspective, if irritant then avoid), cross arm stretch, stretch behind back using towel/belt
- Posterior/inferior glenohumeral joint mobilization
- Continue to progress kinetic chain where appropriate
- Enhance pectoralis minor length
- Strengthen scapular retractors
- Use of ice as necessary
Phase IV - Strengthening Phase (Week 10 – Week 16)
Goals:
- Continue to increaseinternal rotation PROM gradually
- Maintain full non-painful AROM
- Normalise shoulderstrength, joint stability and muscular endurance
- Gradually progress activities with ultimate return to full functional activities
Precautions:
- Strengthening to begin ONLY after approval by surgeon (timing of strengthening may vary on an individual case-by-case basis)
- DO NOT stress the posterior capsule with aggressive overhead strengthening
- Avoid contact sports/activities
Weeks 10-12
- Continue stretching and PROM: IRto 65o at 20o abduction, IR to 75o at 90oabduction, unless otherwise noted by surgeon
- Begin gentle isotonic and rhythmic stabilization techniques for rotator cuff musculature strengthening (open and closed chain)
Weeks 12-16
- Continue stretching and PROM all planes to tolerance
- Continue to progress strengthening programme
- Rehab programme should include sports specific drills where appropriate
Phase V – Return to activity phase (Week 16 - Week 24)
Goals:
- Gradual return to sports activities
- Gradual return to recreational activities
- Gradual return to strenuous work activities
Precautions:
- Do not begin throwing, or overhead athletic moves until 6 months post-op
- Weight lifting: avoid wide grip bench press
Weeks 12-16
- Continue progressing stretching and strengthening programme
- Can begin generalized upper extremity weight lifting with low weight, and high repetitions, being sure to follow weight lifting precautions as above
Weeks 16-20
- Can begin golf, tennis (no serving until 6 months.), etc.
- May initiate a cardio strength programme if appropriate
Criteria to return to sports and recreational activities:
- Surgeon clearance
- Pain free shoulder function without signs of instability
- Restoration of adequate ROM for desired activity
- Full strength as compared to the non-operative shoulder.
Reverse Shoulder Replacement Protocol
Download PDF
Modified from the protocol developed at Boston Shoulder Institute by the
Massachusetts General Hospital and Brigham & Women’s Hospital Shoulder Services.
General Information:
Reverse Shoulder Arthroplasty (RSA) is designed specifically for the treatment of:
- Glenohumeral (GH) arthritis when it is associated with irreparable rotator cuff damage or with glenoid morphology that precludes implantation of a conventional or anatomic Total Shoulder Arthroplasty (TSA)
- Complex fractures
- Revision of a previously failed hemi or TSA in which the rotator cuff tendons are deficient or glenoid bone stock is inadequate for implantation of an anatomic glenoid component.
The rotator cuff is either absent or minimally involved with the RSA function; therefore, the rehabilitation for a patient following the RSA is different than the rehabilitation following a traditional TSA. The surgeon, physiotherapist and patient need to take this into consideration when establishing the postoperative treatment plan.
Important rehabilitation management concepts to consider for a postoperative physiotherapy RSA program are:
- Joint protection: Shoulder extension past neutral and the combination of shoulder adduction and internal rotation should be avoided for 6 weeks postoperatively to minimise the risk of dislocation. The typical dislocation position for RSA is with the arm in internal rotation and adduction in conjunction with extension. Movements such as tucking in a shirt or performing bathroom / personal hygiene with the operative arm or pushing up out of a chair with the operative arm should be avoided, especially in the immediate post-operative phase.
- Deltoid function: Stability and mobility of the shoulder joint is now dependent upon the deltoid and periscapular musculature. This concept is the foundation for the postoperative physiotherapy management for a patient who has undergone RSA.
- Function: As with a conventional TSA, maximize overall upper extremity function, while respecting soft tissue constraints.
- ROM: Potential for range of motion gains should be set on a case-by-case basis, depending upon underlying pathology. Normal/full active range of motion of the shoulder joint following RSA is not typically expected. It is typical for internal rotation, in particular, to be somewhat limited even after full rehabilitation of a successful RSA. This will have been explained to the patient pre-operatively by the surgeon, but may sometimes need to be reinforced by the physiotherapist, in terms of ensuring realistic expectations.
This protocol is intended as a guideline to the post-operative rehabilitation pathway for a patient who has undergone a reverse shoulder arthroplasty (RSA). It is not intended as a substitute for a Chartered Physiotherapist's clinical decision-making regarding how their patient is progressing. Clinical exam findings, individual progress, and/or the presence of post-operative complications. If there are any concerns as to how your patient is progressing please contact Dublin Shoulder Institute.
The scapular plane is defined as the shoulder positioned in 30 degrees of abduction and forward flexion with neutral rotation. ROM performed in the scapular plane should enable appropriate shoulder joint alignment.
Shoulder Dislocation Precautions:
- No shoulder motion behind back. (NO combined shoulder adduction, internal
rotation, and extension.)
- No glenohumeral (GH) extension beyond neutral.
*Precautions should be implemented for 6 weeks post-operatively unless the surgeon specifically advises patient or therapist differently.
Surgical Considerations:
The surgical approach needs to be considered when devising the postoperative plan of care.
- Traditionally the RSA procedure is done via a typical deltopectoral approach, which minimizes surgical trauma to the anterior deltoid.
- Some surgeons perform this procedure via a superior approach, retracting the anterior deltoid from the anterior lateral one third of the clavicle. This allows for superior exposure to the GH joint between the retracted anterior deltoid and the clavicle. Upon surgical closure the anterior deltoid is sutured back to its anatomical location. In these cases early deltoid activity is contraindicated. A variation of the below protocol is recommended for patients who have had a superior approach. These patients should use a sling for 4-6 weeks, should not begin deltoid isometrics for at least four weeks post-operatively, should not begin active range of motion (AROM) flexion for at least six weeks, and should not begin deltoid strengthening for at least 12 weeks post- operatively.
The start of this protocol is delayed 3-4 weeks following RSA as a revision procedure and/or in the presence of poor bone stock based on the surgeon's assessment of the integrity of the surgical repair. In the case of a delayed start to physiotherapy, adjust the below time frames so that day 1 is the first day of physiotherapy for the patient.
Patients are discharged from hospital wearing a shoulder immobiliser (DonJoy Ultrasling III). Patients will attend for a 2 week post-op review before attending with their Chartered Physiotherapist.
Please see above for a video explaining how to correctly wear the shoulder immobiliser.
Progression to the next phase based on Clinical Criteria and/or Time Frames as appropriate.
Phase I – Immediate Post Surgical Phase/Joint Protection (Day 1-6 weeks)
Goals:
- Patient and family independent with:
- Joint protection
- Passive range of motion (PROM)
- Managing shoulder immobiliser
- Getting patient dressed and managing personal bathing
- Assisting with home exercise program (HEP)
- Use of Ice as needed
- Promote healing of soft tissue / maintain the integrity of the replaced joint.
- Enhance PROM.
- Restore active range of motion (AROM) of elbow/wrist/hand.
- Independent with activities of daily living (ADL’s) with modifications.
- Independent with bed mobility, transfers and ambulation or as per pre-admission status.
Acute Care Therapy (Day 1 to 4):
- Active/Active Assisted ROM (A/AAROM) of cervical spine, elbow, wrist, and hand
- Continuous use of Ice for first 72 hours post-operatively, then frequent application
(20 minutes, 4 or 5 x daily)
- Ensure patient is independent in bed mobility, transfers and ambulation
- Ensure proper sling fit/alignment/ use.
- Instruct patient in proper positioning, posture, initial home exercise program
- Provide patient/ family with written home program including exercises and protocol information.
Day 5 to 28:
- Continue all exercises as above
- Begin pendulums at 2 weeks
- Begin PROM in supine at 3 weeks
- Forward flexion and elevation in the scapular plane in supine to 90 degrees.
- External rotation (ER) in scapular plane as indicated by operative findings. If the patient had a repairable subscapularis, ER will be limited to 30o until 6 weeks post op. If the patient did not have a repairable subscapularis (which is not necessary for RSA to function), there will be no limits placed on ER.
- No Internal Rotation (IR) range of motion
- Frequent use of ice (20 minutes, 4 or 5 x daily).
Week 5 to 6:
- Begin sub-maximal pain-free deltoid isometrics in scapular plane (avoid shoulder
extension when isolating posterior deltoid.)
- Progress PROM:
- Forward flexion and elevation in the scapular plane in supine to 120 degrees.
- ER in scapular plane to tolerance, respecting soft tissue constraints.
- Gentle resisted exercise of elbow, wrist, and hand.
- Continue use of Ice.
Criteria for progression to the next phase (Phase II):
- Tolerates shoulder PROM and isometrics; and, AROM- minimal resistance program for elbow, wrist, and hand.
- Demonstrates the ability to isometrically activate all components of the deltoid
and periscapular musculature in the scapular plane.
Phase I Precautions:
- Sling is worn for 4 weeks post-operatively and only removed for exercise and bathing once able. The use of a sling often may be extended for a total of 6 weeks, if the current RSA procedure is a revision surgery. The surgeon will specify this in post-op instructions.
- While lying supine, the distal humerus / elbow should be supported by a pillow or towel roll to avoid shoulder extension. Patients should be advised to “always be able to visualize their elbow while lying supine.”
- No shoulder AROM.
- No lifting of objects with operative extremity.
- No supporting of body weight with involved extremity.
- Keep incision clean and dry (no soaking for 2 weeks)
Phase II –Active Range of Motion Phase (Week 6 to 12):
Goals:
- Continue progression of PROM (full PROM is not expected).
- Gradually restore AROM.
- Pain control as needed
- Allow continued healing of soft tissue / do not over stress healing tissue.
- Re-establish dynamic shoulder and scapular stability.
Week 6 to Week 8:
- Continue with PROM programme.
- At 6 weeks post-op start PROM IR to tolerance (not to exceed 50 degrees) in the scapular plane.
- Begin shoulder AA/AROM as appropriate.
- Forward flexion and elevation in scapular plane in supine with progression
to sitting/standing.
- ER and IR in the scapular plane in supine with progression to
sitting/standing.
- Initiate gentle scapulothoracic rhythmic stabilization and alternating isometrics in supine as appropriate. Minimize deltoid recruitment during all activities / exercises.
- Progress strengthening of elbow, wrist, and hand.
- Gentle glenohumeral and scapulothoracic joint mobilizations as indicated (Grade I and II).
- Continue use of ice as needed.
- Patient may begin to use hand of operative extremity for feeding and light activities of daily living including dressing, washing.
- Where appropriate, patient could be provided with low-level kinetic chain exercises as part of their home exercise program.
Week 9 to Week 12:
- Continue with above exercises and functional activity progression.
- Begin gentle glenohumeral IR and ER sub-maximal pain free isometrics.
Phase II Precautions:
- Due to the potential of an acromion stress fracture, one needs to continuously monitor the exercise and activity progression of the deltoid. A sudden increase of deltoid activity during rehabilitation could lead to excessive acromion stress. A gradually progressive, pain-free programme is essential.
- Continue to avoid shoulder hyperextension.
- In the presence of poor shoulder mechanics avoid repetitive shoulder AROM exercises/activity.
- Restrict lifting of objects to no heavier than a coffee cup.
- No supporting of body weight by involved upper extremity.
Criteria for progression to the next phase (Phase III):
- Improving function of shoulder.
- Patient demonstrates the ability to isotonically activate all components of the
deltoid and periscapular musculature and is gaining strength.
Phase III – Early/Moderate Strengthening (Week 12 +)
Goals:
- Enhance functional use of operative extremity and advance functional activities.
- Enhance shoulder mechanics, muscular strength and endurance.
Phase III Precautions:
- No lifting of objects heavier than 3kg with the operative upper extremity
- No sudden lifting or pushing activities.
Week 12 to Week 16:
- Begin gentle periscapular and deltoid sub-maximal pain free isotonic strengthening exercises. Begin AROM supine forward flexion and elevation in the plane of the scapula with light weights (0.5-1.5 kg) at varying degrees of trunk elevation as appropriate. (i.e. supine lawn chair progression with progression to sitting/standing).
- Progress to gentle glenohumeral IR and ER isotonic strengthening exercises in side lying position with light weight (0.5-1.5kg) and/or with light resistance bands or sport cords.
- Progress to gentle resisted flexion, elevation in standing as appropriate.
- Continue to progress kinetic chain exercises.
Phase IV – Continued Home Program (Typically 4 + months post-op):
- Typically the patient is on a home exercise programme to be performed 3-4 times per week with the focus on:
- Continued strength gains
- Continued progression toward a return to functional and recreational activities within limits as identified by progress made during rehabilitation and outlined by surgeon and physiotherapist.
Criteria for discharge from supervised therapy:
- Able to maintain pain free shoulder AROM demonstrating proper
shoulder mechanics (typically 80 – 120o of elevation with functional ER
of approximately 30o.)
- Able to complete light household and work activities.
Rotator Cuff Repair Protocol
Download PDF
This protocol is intended as a guideline to the post-operative pathway for a patient who has undergone an arthroscopic rotator cuff repair. It is not intended as a substitute for a Chartered Physiotherapist’s clinical decision-making as to how their patient is progressing. Clinical exam findings, individual progress, and/or the presence of post-operative complications will determine progress through the pathway. If there are any concerns as to how your patient is progressing, please contact Dublin Shoulder Institute.
Patients are discharged from hospital wearing a shoulder immobilizer with an abduction pillow (usually a DonJoy Ultrasling IV) and with a home exercise program consisting of AROM for elbow/wrist/hand. Depending on the individual cuff tear, some gentle passive shoulder ROM may also be prescribed. Patients will then attend Dublin Shoulder Institute for their 2-week post-op review where they will be provided with a detailed physio script that they bring to their first appointment with their own Chartered Physiotherapist.
See above for video on wearing the shoulder immobiliser correctly.
Progression to the next phase is based on Clinical Criteria and/or Time Frames as Appropriate.
Phase I – Immediate Post Surgical Phase (Weeks 1-4):
Goals:
- Protect surgical repair and wound/incision sites.
- Manage pain.
- Prevent muscular inhibition.
- Independent for ADL’s with modifications, while maintaining integrity of
Precautions:
- Shoulder immobiliser to be worn at all times – can remove for bathing and any home exercises that may have been prescribed (not all patients will have shoulder ROM exercises prescribed in the first 2 – 4 weeks).
- NO driving.
- NO active range of motion (AROM) of Shoulder
- NO lifting of objects.
- NO shoulder motion behind back.
- NO excessive stretching or sudden movements.
- NO supporting of body weight by hands.
- Keep incision clean and dry.
DAY 1 TO 6:
- Shoulder immobiliser to be worn AT ALL TIMES except for bathing.
- Scapula musculature isometrics; cervical spine ROM.
- Patient education: posture, joint protection, positioning, hygiene, etc.
- Ice for pain relief (Ice Band).
DAY 7 TO 14:
- Continue use of shoulder immobilizer.
- Continue elbow/wrist/hand AROM.
- Continue use of ice for pain relief.
DAY 15-28:
- Continue to wear shoulder immobiliser until end of week 4. **Some patients may need to wear it until end of week 6 depending on extent of repair. See physio script.
- Please refer to physio script from 2-week post-op review for instructions on commencing passive movements in flexion, scaption, ER and IR (scapular plane)
- encourage use of swimming pool where appropriate to aid with passive ROM.
- Continue elbow, wrist, and hand AROM.
- Continue use of ice as needed. Heat can also be used from this stage if advised at 2-week post-op review.
- Pendulum exercises
- to begin 28 days after surgery, no pendulums before this time.
Phase II – Protection Phase (Week 4-10):
Goals:
- Allow healing of soft tissue.
- Do not overstress healing tissue.
- Gradually restore full passive ROM (week 4-5).
- Continue to manage pain.
Precautions:
- NO lifting
- NO supporting of body weight by hands and arms
- NO sudden jerking motions
WEEK 5-6:
- Initiate active assisted range of motion (AAROM) flexion in supine position – if not already commenced as advised by DSI physio or surgeon prior to this.
- Continue progressive passive ROM.
- This ROM should be PAIN FREE.
- Gentle scapular/glenohumeral joint mobilization as indicated to regain full
passive ROM
- Continue previous exercises in Phase I as needed.
- Continue Phase II precautions.
- Initiate prone rowing to neutral arm position.
- Continue use of ice as needed.
- May use heat prior to ROM exercises.
- Continue to encourage pool work for ROM exercises where possible.
- Kinetic chain exercises can commence (bridge; 1 leg bridge, hip hinge in standing).
- ACTIVE ROM can begin before week 6 for some patients – see patient’s individual physio script.
WEEK 6-8:
- Continue AAROM and stretching exercises, including HBB stretch (hand behind back) for internal rotation/posterior capsule.
- Begin rotator cuff isometrics.
- Begin/continue ACTIVE ROM (flexion, scaption)
Phase III – Intermediate phase (week 10-14):
Goals:
- Full AROM (week 10-12)
- Maintain Full PROM
- Dynamic Shoulder Stability
- Gradual restoration of shoulder strength, power, and endurance (after week 12)
- Optimize neuromuscular control
- Gradual return to functional activities
Precautions:
- NO lifting of heavy objects (no heavier than 2 kg)
- NO sudden lifting/ jerking or pushing activities
WEEK 10:
- Continue stretching and passive ROM
- Dynamic stabilization exercises
- No strengthening before week 12, and then only on approval of operating surgeon (patients will attend clinic with surgeon at the 12-week mark & a further, updated physio script will be provided)
WEEK 12:
- Initiate strengthening programme ONLY when full ROM regained and ONLY on approval of operating surgeon (exact timing of introduction of strengthening may vary for individual patients)
-External rotation (ER)/Internal rotation (IR) with Therabands/sport cord/tubing
-ER Side-lying
-Lateral Raises*
-Full Can in Scapular Plane* (avoid empty can abduction exercises)
-Prone Rowing
-Prone Horizontal Abduction
-Prone Extension
-Elbow Flexion
-Elbow Extension
*Patient must be able to elevate arm without shoulder or scapular hiking before initiating isotonics; if unable, continue glenohumeral joint exercises.
WEEK 14:
- Continue all exercises listed above.
- Progress to fundamental shoulder exercises
Criteria for progression to the next phase (IV):
- Able to tolerate the progression to low-level functional activities.
- Demonstrates return of strength / dynamic shoulder stability.
- Re-establish dynamic shoulder stability.
- Demonstrates adequate strength and dynamic stability for progression to higher demand work/sport-specific activities.
- Phase IV – Advanced strengthening phase (week 16-22):
- Goals:
- Maintain full non-painful active ROM.
- Advance conditioning exercises for enhanced functional use of upper extremity.
- Improve muscular strength, power, and endurance.
- Gradual return to full functional activities.
WEEK 16:
- Continue ROM and self-capsular stretching for ROM maintenance.
- Continue progression of strengthening.
- Advance proprioceptive, neuromuscular activities.
WEEK 20:
- Continue all exercises listed above.
- Continue ROM and self-capsular stretching for ROM maintenance.
Phase V – Return to activity phase (week 20-26):
Goals:
- Gradual return to strenuous work activities.
- Gradual return to recreational activities.
- Gradual return to sport activities.
WEEK 23:
- Continue strengthening and stretching.
WEEK 26:
- May initiate interval sport program (i.e. golf, tennis etc.), if appropriate.
Shoulder Replacement Protocol
Download PDF
Modified from the protocol developed at Boston Shoulder Institute by the
Massachusetts General Hospital and Brigham & Women’s Hospital Shoulder Services.
This protocol is intended as a guideline to the post-operative rehabilitation pathway for a patient who has undergone an anatomic total shoulder arthroplasty or a hemiarthroplasty. It is not intended as a substitute for a Chartered Physiotherapist's clinical decision-making regarding how their patient is progressing. Clinical exam findings, individual progress, and/or the presence of post-operative complications will determine progress through the pathway. . If there are any concerns as to how your patient is progressing, please contact Dublin Shoulder Institute.
Patients are discharged from hospital wearing a Shoulder Immobiliser (Don Joy Ultrasling III). Patients will attend for a 2 week post-op review before attending with their Chartered Physiotherapist.
Please see above for a video explaining how to wear the shoulder immobiliser correctly.
Progression to the next phase based on Clinical Criteria and/or Time Frames as appropriate.
Phase I – Immediate Post Surgical Phase:
Goals:
- Allow healing of soft tissue
- Maintain integrity of replaced joint
- Gradually increase passive range of motion (PROM) of shoulder; restore active range of motion (AROM) of elbow/wrist/hand
- Reduce pain and optimise healing process
- Reduce muscular inhibition
- Independent with activities of daily living (ADLs) with modifications while maintaining the integrity of the replaced joint.
Post-Operative Day 1 (POD1 - in hospital):
- Passive forward flexion in supine to tolerance
- Gentle ER in scapular plane with a limit of 30o ER
(Attention: DO NOT produce undue stress on the anterior joint capsule, particularly with shoulder in extension)
- Passive IR to chest
- Active distal extremity exercise (elbow, wrist, hand)
- Pendulum exercises
- Frequent use of ice for pain, swelling and inflammation management
- Patient education regarding proper positioning and joint protection techniques
Early Phase I (out of hospital):
- Continue above exercises
- Begin periscapular musculature isometrics / sets (primarily retraction)
- Continue active elbow ROM
- Continue use of ice for pain and inflammation management
Late Phase I:
- Continue previous exercises
- Continue to progress PROM as motion allows
- Begin assisted flexion, elevation in the plane of the scapula, ER, IR in the scapular plane
- Progress active distal extremity exercise to strengthening as appropriate
Precautions:
- Sling should be worn continuously for 4 weeks
- While lying supine, a small pillow or towel roll should be placed behind the elbow to avoid shoulder hyperextension / anterior capsule stretch / subscapularis stretch. When lying supine patient should be instructed to always be able to visualize their elbow. This ensures they are not extending their shoulder past neutral. This should be maintained for 6-8 weeks post-operatively.
- Avoid shoulder AROM.
- Limit passive ER to 30o until 6 weeks post op.
- NO lifting of objects
- NO excessive shoulder motion behind back, especially into internal rotation (IR)
- NO excessive stretching or sudden movements (particularly external rotation (ER))
- NO supporting of body weight by hand on involved side
- Keep incision clean and dry (no soaking for 2 weeks)
- NO driving for 4 weeks (i.e. until shoulder immobilizer has been discontinued)
Patients should then be instructed to try driving for the first time in their driveway or an empty car park and ensure that they can safely and comfortably control the car before getting back out on the road.
Criteria for progression to the next phase (II):
If the patient has not reached the below ROM, forceful stretching and mobilization/manipulation is not indicated. Continue gradual ROM and gentle mobilization (i.e. Grade I oscillations), while respecting soft tissue constraints.
- Tolerates PROM program
- Has achieved at least 90° PROM forward flexion and elevation in the scapular plane.
- Has achieved at least 30° PROM ER in plane of scapula
- Has achieved at least 70° PROM IR in plane of scapula measured at 30° of abduction
Phase II – Range of Motion, Scapular Strengthening Phase:
(Not to begin before 4-6 Weeks post-surgery to allow for appropriate soft tissue healing)
Goals:
- Restore full passive ROM
- Gradually restore active motion
- Control pain and inflammation
- Allow continue healing of soft tissue
- Do not over stress healing tissue
- Re-establish dynamic shoulder stability
Early Phase II:
- Continue with PROM, active assisted range of motion (AAROM)
- Begin active flexion, IR, ER, elevation in the plane of the scapula pain free ROM
- AAROM pulleys (flexion and elevation in the plane of the scapula) – as long as greater than 90° of PROM
- Begin shoulder sub-maximal pain-free shoulder isometrics in neutral
- Scapular strengthening exercises as appropriate
- Begin assisted horizontal adduction
- Gentle glenohumeral and scapulothoracic joint mobilizations as indicated (traction, scapular glides)
- Initiate glenohumeral and scapulothoracic rhythmic stabilization
- Use of ice for pain and inflammation, as needed.
Late Phase II:
- Progress scapular strengthening exercises
Precautions:
- Wean from sling at 4 weeks post-op
- While lying supine a small pillow or towel should be placed behind the elbow to avoid shoulder hyperextension / anterior capsule stretch
- In the presence of poor shoulder mechanics avoid repetitive shoulder AROM exercises/activity against gravity in standing.
- NO heavy lifting of objects (no heavier than coffee cup)
- NO supporting of body weight by hand on involved side
- NO sudden jerking motions
Criteria for progression to the next phase (III):
If the patient has not reached the below ROM, forceful stretching and mobilization/manipulation is not indicated. Continue gradual ROM and gentle mobilization (i.e. Grade I oscillations), while respecting soft tissue constraints.
- Tolerates P/AAROM, isometric program
- Has achieved at least 140° PROM forward flexion and elevation in the scapular plane.
- Has achieved at least 60+° PROM ER in plane of scapula
- Has achieved at least 70° PROM IR in plane of scapula measured at 30° of abduction
- Able to actively elevate shoulder against gravity with good mechanics to 100°
Phase III – Early Strengthening:
(Not to begin before 8 Weeks post-surgery to allow for appropriate soft tissue healing and to ensure adequate ROM)
Goals:
- Gradual restoration of shoulder strength, power, and endurance
- Optimize neuromuscular control
- Gradual return to functional activities with involved upper extremity
Early Phase III:
- Progress AROM exercise / activity as appropriate
- Advance PROM to stretching as appropriate
- Continue PROM as needed to maintain ROM
- Initiate assisted shoulder IR behind back stretch
- Resisted shoulder IR, ER in scapular plane
- Begin light functional activities
- Include Kinetic Chain exercises (where appropriate)
- Begin progressive supine active elevation strengthening (anterior deltoid) with light weights (0.5-1.5 kg) at variable degrees of elevation.
Late Phase III:
- Resisted flexion, elevation in the plane of the scapula, extension (use theraband/sport cords)
- Continue progressing IR, ER strengthening
- Progress IR stretch behind back from AAROM to AROM as ROM allows
(Pay particular attention to avoiding stress on the anterior capsule.)
Precautions:
- NO heavy lifting of objects (no heavier than 3 kg.)
- NO sudden lifting or pushing activities
- NO sudden jerking motions
Criteria for progression to the next phase (IV):
If the patient has not reached the below ROM, forceful stretching and mobilization/manipulation is not indicated. Continue gradual ROM and gentle mobilization (i.e. Grade I oscillations), while respecting soft tissue constraints.
- Tolerates AA/AROM/strengthening
- Has achieved at least 140° AROM forward flexion and elevation in the scapular plane supine.
- Has achieved at least 60+° AROM ER in plane of scapula supine
- Has achieved at least 70° AROM IR in plane of scapula supine in 30° of
abduction
- Able to actively elevate shoulder against gravity with good mechanics to at least 120°.
Note: (If above ROM are not met then patient is ready to progress if their ROM has plateaued and is consistent with outcomes for patients with the given underlying pathology).
Phase IV – Advanced Strengthening:
(Not to begin before 12 Weeks to allow for appropriate soft tissue healing and to ensure adequate ROM, and initial strength)
Goals:
- Maintain non-painful AROM
- Enhance functional use of upper extremity
- Improve muscular strength, power and endurance
- Gradual return to more advanced functional activities
- Progress weight bearing exercises as appropriate
Early Phase IV:
- Typically patient is on a home exercise programme, to be performed 3-4 times per week.
- Gradually progress strengthening programme
- Gradual return to moderately challenging functional activities.
Late Phase IV (Typically 4-6 months post-op):
- Return to recreational activities and hobbies ( gardening, sports, golf, doubles tennis)
Precautions:
- Avoid exercise and functional activities that put stress on the anterior capsule and surrounding structures. (Example: no combined ER and abduction above 80° of abduction.)
- Ensure gradual progression of strengthening
Criteria for discharge from supervised physiotherapy:
- Patient able to maintain non-painful AROM
- Maximized functional use of upper extremity
- Maximized muscular strength, power, and endurance
- Patient has returned to advanced functional activities
Subacromial Decompression Protocol
Download PDF
Modified from the protocol developed at Boston Shoulder Institute by the Massachusetts General Hospital and Brigham & Women’s Hospital Shoulder Services.
Arthroscopic Subacromial Decompression Protocol:
This protocol is intended as a guideline to the post-operative rehabilitation pathway for a patient who has undergone an arthroscopic subacromial decompression. It is not intended as a substitute for a Chartered Physiotherapist's clinical decision-making regarding how the patient is progressing. Clinical exam findings, individual progress and/or the presence of post-operative complications will determine progress through the pathway. If there are any concerns as to how your patient is progressing, please contact us at the Dublin Shoulder Institute.
After isolated subacromial decompression, patients are discharged from hospital with a sling to be worn for comfort only. Unless otherwise specified, the patient should wean out of the sling in the days following surgery and be completely out of it by one week post-operatively at the latest.
Other surgical procedures may be performed alongside subacromial decompression - please refer to the postoperative physiotherapy prescription.
Phase 1: Protective healing and restore movment (1-2 weeks)
Goals:
- Reduce pain/inflammation
- Minimize stress to healing structures
- Restore non-painful range of motion (ROM)
- Minimise shoulder muscle atrophy and muscle inhibition
- Improve postural awareness
- Independent with activities of daily living (ADLs)
- Wean from sling ASAP.
Range of Motion: - Passive range of motion (non-forceful flexion and abduction)
- Active assisted range of motion (AAROM)
- Active ROM
- Pendulums
- Pulleys
- Cane exercises
- Prescribed stretches
- Proprioceptive Neuromuscular Facilitation (PNF)
- Thoracic Spine mobility - Rotation stretches.
Strengthening: - Isometrics: scapular musculature, deltoid, and rotator cuff as appropriate
- Kinetic Chain exercises (Bridge, 1 leg bridge, Hip Hinge in standing)
NOTE: Do not commence any upper limb functional strength movements (push/pull) until FULL AROM (flexion, abduction, external rotation) has been achieved and is maintained.
Modalities:
Manual therapy- Thoracic spine PIVM's to improve thoracic spine mobility, GH joint traction for pain modification (Gd I/II from 7 days post-op if comfortable for patient)
• Light massage/ release of deltoid and latissimus dorsi
• Ice
• Heat/ice contrast: to reduce pain and swelling a heat/ ice contrast can be used from 7 days post-op.
Criteria for progression to Phase 2:
- Full active and passive ROM
- Minimal pain and tenderness
Precautions:
- Avoid pure shoulder abduction (both active and passive) to avoid unnecessary compression of subacromial structures, work in scaption instead.
- Avoid creating or reinforcing poor movement patterns, such as excessive scapulothoracic motion with upper extremity elevation
Phase 2: Intermediate Phase (2-6 Weeks)
Goals:
- Regain and improve muscular strength (ONLY after full ROM has been achieved)
- Normalise arthrokinematics
- Improve neuromuscular control of shoulder complex
Exercises: - Strengthen shoulder musculature- add resistance with dumbells, resistance bands and body weight.
- Include 'Push/Pull' exercises. Consider strengthening in all planes of motion.
- Strengthen scapulothoracic musculature- by including Row or Pull type exercises
- Initiate upper extremity endurance exercises
- Continue and progress Kinetic chain exercises.
- Incorporate upper limb strengthening with lower limb exercises.
Manual Treatment: - GH joint mobilisation to improve/restore arthrokinematics
- GH joint mobilisation for pain modulation
Modalities:
Ice as needed.
Criteria for Progression to Phase 3:
- Full painless ROM
- No pain or tenderness on examination
Phase 3: Dynamic (Advanced) Strengthening Phase (from 6 weeks)
Goals:
- Improve strength, power and endurance
- Improve neuromuscular control
- Prepare patient to begin throwing and other overhead activities relevant to occupation or sport.
Emphasis of Phase 3:
- High Spees, high energy strengthening exercises
- Eccentric exercises
- Diagonal patterns (use resistance band or dumbells)
Exercises:
- Include push/pull exercises in supine, standing (chest press/ overhead press, bent over row, horizontal row, lat pull down, band press)
- Progress resistant band exercises to 90/90 position (shoulder abduction / ER) for internal rotation and external rotation (slow/fast sets). Incorporate kinetic chain where appropriate (lunge stance, 1 leg stance)
- Plyometrics for rotator cuff
- Diagonal chop exercises
- Isokinetics – high plank holds (with arm or leg lift)
- Continue endurance exercises
Superior Capsular Reconstruction Protocol
Rehabilitation Guidelines following Superior Capsule Reconstruction (SCR) of the Shoulder.
Download PDF
What is SCR?
SCR is an anatomic reconstruction of the Superior Capsule of the Shoulder (Mihata et al 2012). It is indicated in patients with irreparable tears of the rotator cuff and where there is evidence of a defect in the superior capsule, with no arthritis in the glenohumeral joint.
In patients who have a large, full-thickness tear of the rotator cuff the humeral head may move superiorly in the glenoid during arm elevation. This disrupts the force couple that exists between the deltoid muscle and the rotator cuff, and can present clinically as the patient “hitching” their shoulder.
SCR can restore glenohumeral joint kinematics by helping to centre the humeral head in the glenoid fossa, establishing a stable fulcrum and allowing the deltoid and the cuff to function more effectively. This helps the patient with elevation of their arm.
While patients may not regain complete strength without a native rotator cuff, initial clinical studies on SCR show that patients can achieve significant reduction in pain and improvement in function.
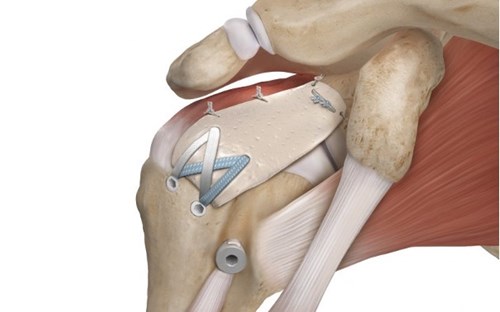
THE GRAFT:
We currently use a porcine xenograft dermal extracellular graft (Arthrex DX Matrix) to reconstruct the superior capsule of the shoulder. Biological grafts are preferred over synthetic grafts because they contain collagen thus natural cell interactions such as proliferation and migration occur.
A successful post-operative outcome is dependent on a successful healing process, which consists of the initial inflammatory phase. The following occurs:
- Fibroblasts must penetrate the collagen matrix within the biological graft.
- Cell Proliferation/degradation occurs , essential for host acceptance of biological graft.
- Remodelling/maturation phase – cells, blood vessels and collagen organise where the fibres align along different tension lines to achieve overall tensile strength of the graft.
IF REMODELLING DOES NOT OCCUR PROPERLY, TISSUE DEGRADATION AND REJECTION OF THE GRAFT COULD OCCUR.
REHABILITATION PRINCIPLES
Three main principles are:
- Optimise graft healing as part of a conservative rehab approach.
- Deltoid re-education.
- Collaboration between surgeon, therapist and patient.
OPTIMISE GRAFT HEALING via a conservative approach. Evidence suggests that the grafts undergoes significant remodelling and becomes weaker before it gets stronger.
DELTOID RE-EDUCATION - The deltoid plays key role in the rehab process of patients who have undergone SCR as the deltoid is considered the prime mover of the arm in the absence of a complete, functioning rotator cuff.
COLLABORATION SURGEON/THERAPIST/PATIENT- close communication with the surgeon is essential for a successful post-operative outcome. Clinicians also need to constantly monitor the patient’s expectations by explaining the time lines of expected benefits and recovery.
REHAB PHASES
Patients are discharged from hospital wearing a shoulder immobiliser
(DonJoy Ultrasling III) and with a home exercise programme consisting of
AROM for elbow/ wrist / hand. Patients will then attend for a 2-week post-op
review before attending with their Chartered Physiotherapist.
A video explaining how to correctly wear the shoulder immobiliser can be found here: https://www.dublinshoulder.com/services/shoulder-surgery/
PHASE 1: PROTECTIVE PHASE 0-6 weeks (patient in sling, initial inflammatory phase occurring - healing the graft).
Goals:
- It is beneficial for the patient to have a clear understanding on the rationale of the surgery and the rehabilitation process.
- Ensure fine balance between protecting graft and reducing post-op stiffness.
- Ensure patient compliance with sling and home exercise program.
- Ensure patient is comfortable, managing any pain and sleeping well. (Reassure the patient that it may take some time to be comfortable at night and sleeping normally, this is an expected part of the initial post-operative period)
Precautions:
- Arm is to remain in sling, and removed only for HEP and washing/dressing.
- NO Active ROM of the shoulder. No hand behind back or across body.
- NO supporting of body weight with hands.
- NO driving.
Treatment & Management:
- 2 week post-op check with surgeon for wound check (absorbable stitches are used) and physiotherapy instructions.
- Patient is to wear sling for 6 weeks.
- Inform patient re: timeframes of recovery and functional improvements.
- Ice (10 min, 3-5 x daily) and pain relief as prescribed.
- PROM may commence before 6 weeks to prevent post-op stiffness. Please refer to patient Physiotherapy Prescription note from Dublin Shoulder Institute.
Treatment Considerations:
- Sensorimotor control should start early in the rehab and progress through the phases.
- Assess for Pectoralis dominance. Patients will often be in a protracted shoulder position and have an increase in resting tone of the muscles (observable or by palpation).
PHASE 2 : INTERMEDIATE PHASE ( 6 weeks – 4 months, Graft incorporation and Revascularisation phase).
GOALS:
- Restore Functional AROM ( Flexion, Scaption, ER, IR)
- Establish basic rotator cuff and scapular neuromuscular control, in pain free ROM.
- Regular physiotherapy required to guide patient through this rehab phase.
PRECAUTIONS
- NO exercise/ activity that increases pain
- NO specific cuff strengthening exercises until 12 weeks.
- NO bands/ heavy lifting/ weights to be used until 12-weeks.
- NO supporting of body weight by hands or arms.
Treatment & Management:
- Regular physiotherapy is required to guide patients through this rehab phase.
- Start with Active Asssisted ROM and progress to Active ROM through range, focusing on scapular control.
- GH joint and scapular mobilisations as indicated to regain ROM.
- Closed-chain stability exercises can start with wall push-ups.
- Can begin rotator cuff isometric exercises below shoulder height.
- Commence Anterior Deltoid Re-education programme*
- Serratus Anterior Activation: patient in supine, arms at 90 degrees flexion and full scapular protraction.
- Pool session are beneficial - supervised hydrotherapy session or self-directed PROM in the pool.
- End of Phase: Weight shifts and perturbations will improve static control through compressive forces acting on GH joint. Start in incline position and gradually lower to quadruped on floor.
- End of Phase: Kinetic chain exercises for strengthening posterior chain – where appropriate.
- Review with surgeon at 12 weeks post-operatively.
By end of this Phase, patient should be able to carry out light to moderate functional activity at waist and shoulder height, have minimal pain and be sleeping well.
Considerations:
Ensure exercises are goal orientated with proprioceptive, functional and dynamic elements.
Some patients may have difficulty recruiting the deltoid as the prime mover of the shoulder. Biofeedback, surface EMG, verbal/tactile cues and tape can be used to help patients.
*www.shoulderdoc.co.uk/article/1028 is an example of an evidence-based deltoid re-education program (based on study by Levy et al, 2008).
PHASE 3: STRENGTHENING phase (4-6 months). Remodelling phase of healing where collagen fibres are laid down to achieve tensile strength of the graft.
GOALS:
Rehab to include a structured and progressive strengthening program for the deltoid, remaining rotator cuff and scapular stabilisers.
Patients to return to more physically demanding work and activities.
Precautions:
- No lifting of heavy objects
- No contact sport.
Treatment & Management:
- Integration of the kinetic chain into Home Exercise Program.
- Progress strengthening program with body weight/ free weights/ resistance bands.
- Activate posterior rotator cuff through available range with band. Start in supine position and progress to standing.
- Progress through program for deltoid re-education.
- Progress closed chain exercises (use Swiss Ball/ Pilates Ball to increase co-contraction of deep stabilisers/ improve dynamic shoulder stability/scapular control).
- Incorporate sensorimotor control exercises.
- Dynamic bear hug (with resistance band) for Serratus anterior, Trapezius, Rhomboids). Can also be done in a lunge hold position to bring in kinetic chain.
- Exercises with weight transference – push ups at wall/ on incline and lift good hand away.
- Thoracic rotation and extension exercises
- Advise of injury prevention strategies and continued benefit of regular cardio-vascular exercise.
- Review with surgeon at 6 months post-op.
Treatment & Management:
- Integrate the kinetic chain in assessment and treatment plans. Consider Lumbo-pelvic hip complex (LHPC) and its importance in force production for upper limb function. A stable proximal base will enhance distal arm function. (https://www.aspetar.com/journal/viewarticle.aspx?id=198#.YCWxFqecY_U)
- Encourage good postural habits and maintain available range of thoracic extension: 15 degrees of thoracic extension is required for pain free shoulder elevation.
PHASE 4: End stage Rehabilitation (6-12 months).
GOALS:
- Encourage patients to maintain their exercise programme and an active lifestyle up to 12 months post-operatively and beyond.
- Provide an individualised rehab program for greater upper Llmb function.
Long term rehab program should include :
- Strengthening exercises for return to full functional activities.
- Enhanced proprioceptive and neuromuscular control programme.
- Exercises in overhead position.
- “Push-up Plus” for Serratus anterior.
Contact with patient at 12 and 24 months post-operatively for outcome scores.
If you or your physiotherapist have any questions or concerns during your post-operative rehabilitation, please do not hesitate to contact us.